Cervical osteochondrosis is a chronic disease caused by degenerative changes in the intervertebral discs of the neck. As the disease progresses, the surrounding structures become involved in the pathological process, which causes the development of a number of unpleasant symptoms. Treatment of the disease is complex, conservative and includes taking medications and non-drug methods.
Causes
The exact reasons are unknown. The theory that the development of the disease is associated with age-related changes has not been confirmed, since today this pathology is diagnosed even in adolescents.
Factors that can trigger the development of the disease include:
- low physical activity, sedentary lifestyle;
- mechanical neck injuries;
- sedentary work with high static load on the cervical spine;
- uncomfortable mattresses and pillows;
- obesity;
- circulatory disorders;
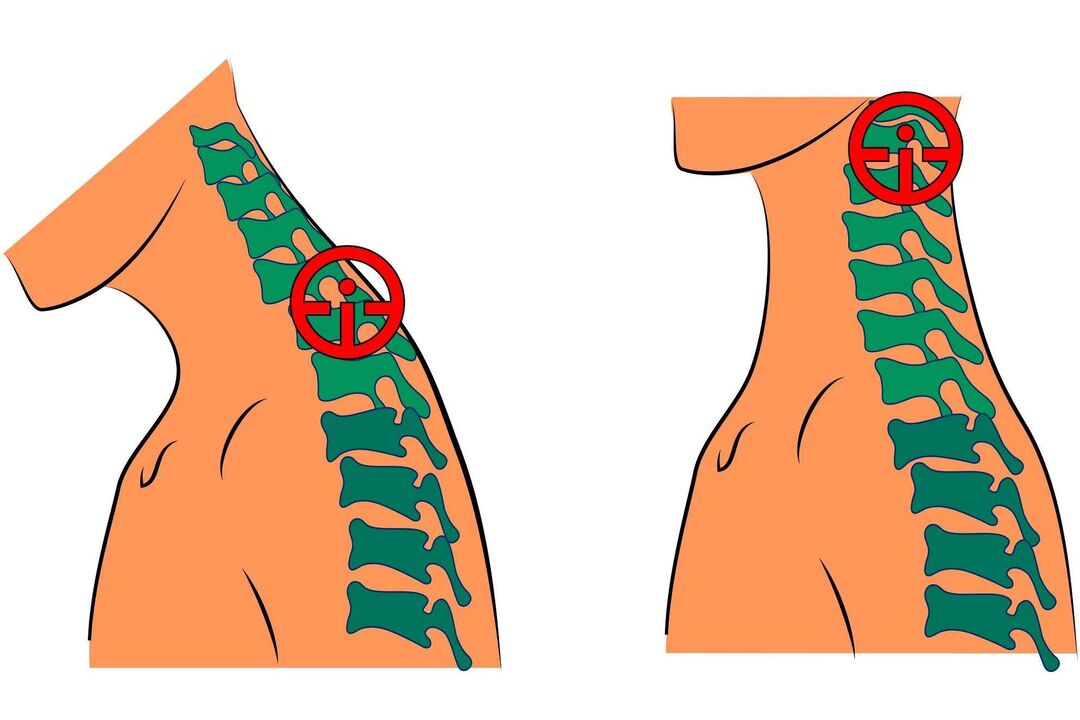
- scoliosis and other posture defects;
- connective tissue dysplasia;
- Metabolic disorders.
Syndromes and symptoms

Symptoms of cervical osteochondrosis do not appear immediately. For a long time, the disease can develop asymptomatically or disguise itself as other pathologies. The most common signs of cervical osteochondrosis are:
- tinnitus - usually occurs when changing position after a long stay in a stationary position;
- dizziness - the patient periodically feels as if objects are beginning to rotate in front of his eyes;
- pain in the neck, back of the head - the intensity of pain depends on the degree of pathological changes;
- feeling of lack of air - the patient cannot breathe deeply;
- visual impairment - occurs in later stages;
- nausea, vomiting - are also associated with impaired blood supply to parts of the brain due to compression of key arteries by deformed discs;
- sore throat, dry throat, foreign body sensation;
- pressure changes poorly controlled by medications;
- numbness of fingers;
- shoulder pain.
In addition to the general clinical signs, several characteristic syndromes can be distinguished:
Vertebral:
- pain when turning the neck;
- reduced mobility;
- X-rays show signs of damage to the vertebrae and discs.
Cardiac:
- burning and pain in the chest;
- increased fatigue, weakness without cause;
- tachycardia.
Vertebral artery. This syndrome results from a narrowing of the vertebral artery, which supplies blood to the brain. Manifested by tinnitus, dizziness and blurred vision.
Koreshkovy. This occurs due to pinching or compression of the nerve roots that exit the cervical spine.
Steps
Stages of the disease:
- The patient feels slight discomfort in the neck. The intervertebral discs begin to lose their stability.
- Pain appears. The discs become deformed, the destruction of the annulus fibrosus begins, and the vertebrae move closer to each other.
- Neck movements are limited. When turning the head, nausea and dizziness may occur. A constant lack of blood to the brain leads to symptoms such as lethargy, weakness, decreased performance and fatigue. The discs become thinner, the vertebrae begin to rub against each other, the annulus fibrosus is destroyed and intervertebral hernias form.
- The neck area is immobilized, the blood supply to the brain is completely disrupted. To correct this condition, the patient must constantly take special medications. The vertebrae begin to fuse together.
Diagnostic
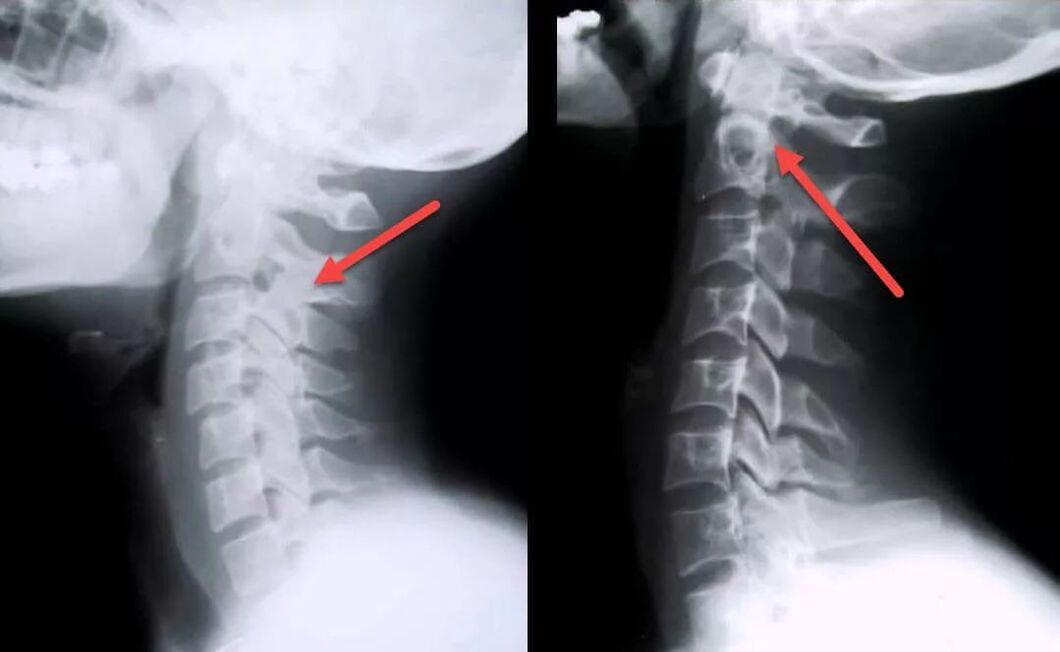
Diagnosis can be difficult due to the nonspecific clinical picture and the high variability of possible symptoms. The patient may need the help of several specialists at once (surgeon, neurologist, cardiologist, vertebrologist, orthopedist and others).
During the appointment, the doctor listens to the patient's complaints, collects anamnesis, conducts an examination and makes a preliminary diagnosis.
To confirm this, the following may be prescribed:
- blood test;
- MRI of the neck - allows you to identify pathological changes even at the initial stage of the disease, when the clinical manifestations are not yet too pronounced; with the help of this study, you can assess the current state of the vertebrae, discs, identify the presence of deformations, osteophytes, compression of nerves and blood vessels;
- Dopplerography of the cervical arteries - allows you to assess the degree of compression and damage to blood vessels, the speed of blood flow;
- myelography using contrast - allows you to identify pinched nerves;
- ECG - carried out for the differential diagnosis of cardiovascular diseases.
Treatment
Drug treatment includes taking the following groups of drugs:
- NSAIDs. Effectively relieves inflammation, pain and swelling. These are means of symptomatic therapy that do not affect the causes of the disease. NSAIDs can be used in short courses of 10 to 14 days.
- Angioprotectors, means of accelerating blood flow. Improves cerebral circulation, protects blood vessels from damage.
- Glucocorticoids. Effectively relieves pain and nerve compression. Medicines in this group have many side effects and should only be taken as prescribed by a doctor if NSAIDs and pain relievers are not effective.
- Chondroprotectors. Improves the health of intervertebral discs, influencing the causes of disease. They inhibit the destruction of cartilage tissue and improve the shock absorption properties of the discs.
Non-drug treatment may include the use of the following techniques:
- Exercise therapy. Regular training strengthens muscles and relieves spasms. It is recommended to take courses (at least at the initial stage) under the guidance of a specialist.
- Manual therapy. Neck muscle spasms are one of the main causes of pain related to this condition. Correctly performed manual therapy helps to eliminate spasms, compression of blood vessels and nerves. As a result, the nutrition of the discs improves, cerebral circulation is normalized and the pain disappears.
- Kinesio recording. The application of special tapes relaxes muscles, relieves spasms, swelling, inflammation and at the same time maintains the spine in a physiologically correct position.
- Orthopedic devices. To minimize the load on the cervical spine, it is recommended to use orthopedic mattresses and pillows for sleeping. Additionally, some patients are recommended to wear a special device (Schanz collar) that fixes the neck in the correct position.
- Massage. An effective remedy for the cervical form of the disease. Perfectly relieves swelling, pain, congestion, improves local blood circulation, relieves muscle spasms. Do not massage if you experience sharp neck pain.
- Physiotherapy. Another effective technique. The sessions take place in class, several times a year. This allows you to get rid of unpleasant symptoms, relieve muscle spasms and slow down the progression of the disease. For the treatment of cervical osteochondrosis, laser therapy, magnetic therapy, mechanotherapy, traction therapy, hydromassage, UVT and mud therapy are most often used.
If conservative treatment does not give results and the disease continues to progress, surgical treatment may be prescribed.
- operations to remove intervertebral hernias;
- removal of the vertebral arch or spinous processes results in decompression of the roots of the spinal cord;
- removal of part of the disc nucleus to repair a herniation.
The decision on how to treat the disease is made by the doctor individually for each patient. Self-medication is prohibited and can lead to the development of a number of complications.
Complications

If the disease is neglected, the following complications may develop:
- VSD;
- lack of oxygen to the brain;
- high blood pressure;
- blurred vision, retinal dystrophy;
- respiratory spasm;
- violation of the act of swallowing due to dysfunction of the esophagus;
- dysfunction of the thyroid gland;
- cramps and numbness of the neck muscles;
- chronic upper body pain that is not relieved by painkillers;
- hormonal imbalances.
Prevention
To minimize the risk of developing the disease, you must adhere to the following recommendations:
- maintain posture;
- properly equip the workplace to avoid neck strain;
- Healthy food;
- stop smoking and drinking alcohol;
- avoid neck injuries;
- move more, exercise;
- do not overcool;
- control weight;
- sleeping on a special orthopedic mattress and pillow;
- do gymnastics regularly to avoid the development of congestion;
- prevent curvature of the spine;
- regularly take massage courses to improve blood circulation and relieve congestion;
- do not sit for a long time in a position with your head tilted forward;
- If you feel discomfort in the neck area, you should make an appointment with a specialist and undergo an examination, this will help identify possible changes in the discs at an early stage, which will greatly facilitate treatment and improve the prognosis.






















